Morning Sickness & Dehydration: Break the Cycle with Safe Hydration Tips 2025
November 1st, 2025 | Nausea, Pregnancy
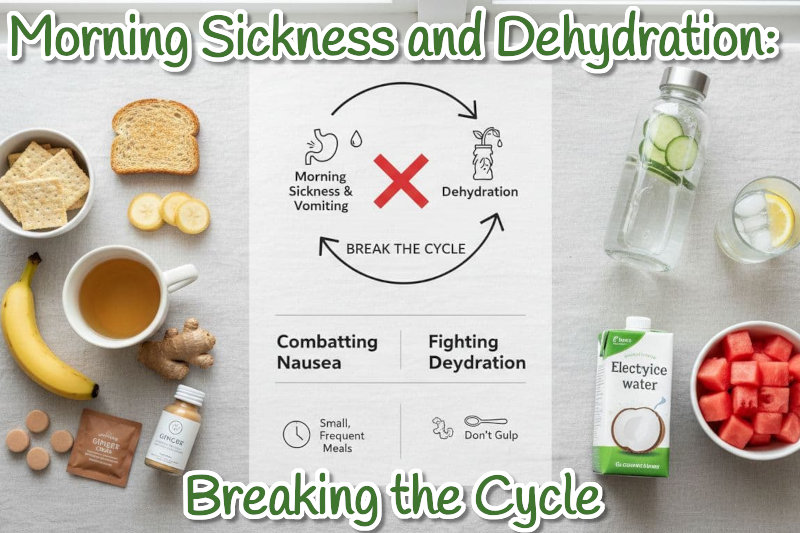
Queasy the moment you wake up, yet the thought of sipping water turns your stomach? You are not alone. Morning sickness and dehydration can trap you in a loop that feels endless. Nausea makes it hard to drink, low fluids make nausea worse. The result can be dry mouth, dark pee, dizziness, and a tired fog that never lifts.
This guide explains why the cycle happens in simple terms, what signs to watch for, and hydration tactics that actually stay down. You will also get an easy daily plan you can follow today, plus when to call your doctor. The goal is calm, steady progress, not perfection. Small sips, light snacks, and a few smart tools can help you feel human again.
Why morning sickness and dehydration feed each other
Your body needs fluids and electrolytes to keep digestion moving and nerves firing. When you vomit or cannot drink, you lose both. That loss dries out your mouth and gut, which can irritate the stomach lining. An irritated stomach sends stronger signals to the brain’s nausea center. The brain then ramps up queasiness, and the urge to vomit grows. It is a loop that feeds itself.
Hormone shifts in early pregnancy add fuel. Rising hCG and estrogen can heighten smell sensitivity and slow stomach emptying. Food stays in the stomach longer, which can increase the chance of nausea. If you are also low on sodium and potassium, the stomach and intestines become more twitchy, and the brain is more sensitive to motion and smells. Even mild dehydration can tip the balance.
Early signs stand out once you know them. Darker urine, a dry or sticky mouth, headaches, dizziness, a fast heartbeat, and heavy fatigue all signal low fluids. If you see these, act now. The fix is not a big glass of water, since that can trigger a wave of nausea. The fix is small, steady sips with some electrolytes. A little at a time helps the gut relearn calm.
You can break the loop with simple steps. Replace fluids and electrolytes in tiny amounts, keep snacks easy and frequent, and use gentle nausea aids. Progress builds fast when you keep it steady and small.
What causes pregnancy nausea and vomiting?
Common drivers include rapid hormone changes, mainly hCG and estrogen, a more sensitive stomach, slowed digestion, and strong smells. Nausea often peaks in the first trimester, though it can appear any time of day. Stress, fatigue, and an empty stomach can make it worse. The pattern is different for everyone, which is why testing small changes helps you find your sweet spot.
Early signs of dehydration you should not ignore
Watch for darker urine, a dry mouth, headaches, dizziness, a fast heartbeat, and feeling very tired. A simple home check is urine color. Pale yellow is the goal. If it looks like apple juice, you likely need more fluids. Do not wait until you feel faint. Start sipping and add electrolytes as soon as these signs show up.
When nausea becomes serious
Call your healthcare provider if you see red flags for hyperemesis gravidarum. These include vomiting more than three times a day, losing weight, being unable to keep liquids down for 24 hours, very dark urine or no urine, confusion, severe belly pain, or blood in vomit. You deserve support and treatment. Urgent care or your obstetric team can help you feel better and stay safe.
The simple science of the cycle
- Vomiting and poor intake lower fluids and electrolytes.
- Low fluids slow digestion and irritate the stomach.
- The stomach gets queasier, which triggers more nausea.
The key is simple. Replace fluids and electrolytes in small, steady amounts, not all at once. Gentle, frequent intake gives your stomach time to reset.
Hydration tactics that actually stay down
When your stomach is on edge, strategy beats willpower. Think in sips, not gulps. Aim for a balance of water and electrolytes. Play with temperature and flavor to find what you can tolerate. Time your sips between meals, and keep the air cool and fresh. Safe over-the-counter aids may help, but talk with your provider first.
Work in short cycles. Sip for 10 minutes, rest for 10 minutes, repeat. Match fluids with easy snacks to calm acid and steady blood sugar. Track what works for three days. Keep the winners, cut the rest.
Sips that stick: fluids and electrolytes
Use an oral rehydration solution or a low sugar electrolyte drink. Start with 1 to 2 tablespoons every 5 to 10 minutes. Increase as it feels safe. Ice chips and crushed ice can be easier than liquid. You can make a simple ORS at home with clean water, a small pinch of salt, a little sugar, and a splash of citrus if you tolerate it. Steady, small intake beats big gulps that bounce right back.
If you prefer a ready option, explore Essential Products for Relieving Pregnancy Nausea like vitamin B6 and ginger that many find gentle on the stomach: https://threelollies.com/pregnancy-nausea-relief/
Cool, sour, and salty can settle the stomach
Very cold water can feel more tolerable. Try lemon or lime in water, ginger tea cooled with ice, or popsicles. Brothy soups offer both fluids and sodium. Many people find sour and salty flavors calm queasiness and help restore electrolytes. Test a few options and note which ones feel best at different times of day.
Eat to ease nausea, not fight it
Keep foods plain and simple. Dry crackers, toast, rice, bananas, applesauce, yogurt, eggs, and smoothies with protein are good choices. Pair carbs with light protein to steady blood sugar. Eat small snacks every 2 to 3 hours, rather than large meals. Keep a snack by the bed for a few bites before you sit up in the morning. A warm belly is happy; avoid very hot, heavy, or greasy foods early in the day.
Nausea relief tools you can use now
Evidence-based aids include vitamin B6 within doses your provider recommends, and doxylamine at night if your provider agrees. Many find acupressure wrist bands, fresh air, and gentle breathing helpful. Ginger can soothe, and some prefer lozenges because they are easy to keep down. If you want a gentle option with flavor, try All-Natural Lollipops for Morning Sickness that many use during travel, work, or rest: https://threelollies.com/preggie-products-for-morning-sickness/
Always check with your clinician before starting medicines or supplements.
Your simple daily plan to break the cycle and keep it from coming back
A routine takes guesswork off your plate. Use short steps you can repeat, then add backups for tough moments. Pay attention to patterns, not perfection. Adjust what you sip, how often you snack, and how cool the room is. Keep supplies within reach so you can act before symptoms spike.
Morning starter routine
Set up a bedside kit. Include water in a covered bottle, a small ORS, and dry crackers or pretzels. On waking, take 3 to 4 small bites before sitting up. Sip 1 to 2 tablespoons of fluid. Sit and breathe for 5 minutes, then stand. Skip hot, strong smelling foods early. If you can, open a window or use a fan for fresh, cool air.
Midday survival kit
Carry a refillable bottle and plan to sip every 15 minutes. Set phone reminders so you do not forget. Pack small salty snacks and a sour or ginger candy. Keep a spare bag just in case. Eat a light snack every 2 to 3 hours. If a smell triggers you, step outside or switch to cold foods with mild odors. For a ready-to-go stash that fits in a bag, consider a Preggie Gift Box for Nausea Relief so you have gentle flavors on hand: https://threelollies.com/product/preggie-gift-box/
Evening wind-down for better sleep
Keep dinner mild and early. Think soup, rice, or eggs with toast. Take slow sips after dinner, not large drinks at once. Prop your head with pillows so your stomach sits lower than your throat. Prepare your bedside kit again. Many people sleep better with a light protein snack before bed, like yogurt or a small smoothie.
Track, tweak, and talk to your provider
Use a simple log with three columns: time, what you ate or drank, and how you felt. Add any triggers you notice. After 3 to 5 days, keep what works and drop what does not. If you cannot keep fluids down, call your provider. Ask about vitamin B6, doxylamine, prescription anti-nausea options, or IV fluids if needed. You deserve relief, and help is available.
Conclusion
Tiny sips, light snacks, and simple routines can stop the spiral that links nausea and dehydration. Progress often comes from quiet changes that add up. Be kind to yourself, rest when you can, and seek help if warning signs show up. Start today with a short list: set up a bedside kit, mix a basic ORS, choose two safe snacks, and set sip reminders. Small steps, taken often, protect your energy and your hydration.
Recent Posts
- Welcoming Longer Days: A Spring Adventure for Little Ones
- Combating Nausea with Aromatherapy – Essential Oils for Chemotherapy Patients
- Finding Your Calm: Relaxation Techniques for New Parents
- Sip Your Way to Relief: Hydration & Bland Drinks for Chemotherapy Nausea
- Surviving Valentine’s Day: A Gentle Guide for the Morning Sickness Warrior
Categories
- All-Natural (4)
- Blog (47)
- Cancer (80)
- Diet (15)
- Holidays (27)
- Lifestyle (69)
- Motion Sickness (44)
- Nausea (107)
- New Mothers (43)
- Oncology Testimonials (3)
- Prebiotics (1)
- Preggie Products (11)
- Preggie Testimonial (24)
- Pregnancy (160)
- Queasy Products (7)
- Queasy Testimonial (17)